5-year strategic plan to uplift recurring revenue by 80% through organic growth within four years
Outcomes
Strategic Organic Growth Development & Implementation Planning
- Identified multiple growth pathways to reach 80% revenue growth within four years
- Developed a balanced framework of win strategies to drive incremental revenue and EBITDA growth
- Generated a 5-year strategic plan, go-to-market launch and implementation roadmap to capture the identified incremental income
Our Client
Is a leading specialist provider of medical consumables in the UK. They have a strong presence in both primary and community care and work with hospitals to improve care delivery and patient outcomes
Background
Curzon was tasked with developing a 5-year strategic plan for a leading distributor of medical consumables in the UK, who were faced with significant changes in the largest customer segment, leading to a material decline in client revenues and EBITDA fell below business case targets
Testimonial
“Curzon’s strategic insight and expertise were evident from the outset. We engaged them to craft a comprehensive 5-year strategy and financial plan, a task that demanded an intricate understanding of our industry’s dynamics, as well as the ability to chart a course through a rapidly evolving healthcare landscape. The Curzon team demonstrated an exceptional knack for identifying opportunities that aligned with our organisational goals, while also addressing potential challenges that lay ahead“.
Managing Director, Leading UK Medical Consumables Distributor
Curzon Approach
- Sized the UK medical consumables by market segment (Private acute, NHS, Care homes)
- Created a vision for the organisation in collaboration with the client senior leadership team
- Shortlisted target segments to drive organic growth
- Developed win strategies, differentiated value propositions and business model options for each segment
- Identified approaches to extend treatment and care pathways into a patient’s home
- Developed a 5-year financial plan including revenue projections and investments required
- Developed a strategic sourcing business case leveraging GPO model
CASE STUDIES
Read some of the client problems we have solved!
Scalable strategy for growth at a UK private hospital group to unlock self-pay revenue
Outcomes
Driving self-pay growth through a data-led go-to-market strategy
- Identified a £67m revenue opportunity by producing a detailed, location-specific market model
- Brokered a strategic partnership which alone is forecasted to generate up to £10m in additional self-pay revenue
- Reduced NHS wait times for elective procedures by redirecting PMI-ineligible patients to private care
Our Client
A leading healthcare provider group in the UK and has a large network of hospitals, fitness and wellbeing centres. They take pride in collaborating with all parts of the health service and not only provide treatment but also focus on preventive health
Background
In response to rising NHS wait times and increasing demand for private care, a leading private hospital group set out to expand its self-pay offering, and sought a strategic partner to drive this growth and wanted to leverage Curzon’s expertise in healthcare strategy
Testimonial
Curzon’s team demonstrated exceptional analytical acumen, providing valuable market insights that has helped us define our self-pay strategy.
Hospital Commercial Director, Leading Healthcare Provider Group
Curzon Approach
- Built a granular, hospital-level revenue model which integrated NHS wait list data with socioeconomic and financial assessments
- Initiated a first-of-its kind smart distribution partnership between the hospital group and broker to covert PMI-declined leads into self-pay patients, creating a new scalable growth channel
- Identified and addressed pain points in the customer journey, including recommendations to improve pricing transparency, digital lead capture and broker confidence
- Proposed enhancements to the value proposition and operational improvements to boost lead conversion and brand perception
- Created a business case to recommend a strategic partnership
CASE STUDIES
Read some of the client problems we have solved!
From one-size-fits-all to specialist rewards: Curzon builds a smarter fee structure for a private medical insurer
Outcomes
The UK’s first, data-driven, value-based reimbursement fee structure
- Crafted a should-cost model encompassing key factors: surgical time, variations based on specialism, surgeon expertise, clinical risk cost, and admin costs
- Delivered benchmarking insights showing client reimbursements compared to market averages, and specifically against another larger insurer
- Compiled a comprehensive report highlighting key findings, outlining urgent need for changes, and providing an initial should-cost model design
Our Client
Is a top 4 private medical insurance provider in the UK with a global footprint. They deliver personalised health and wellbeing services to both individuals and businesses, with a strong emphasis on enhancing healthcare outcomes
Background
Consultants complain about the client’s current reimbursement structure for surgeons and anaesthetists, citing rising practice costs and other unaddressed factors
- Current fee structures do not reflect specialism levels, patient complexities, or actual procedure lengths
- A “one-size-fits-all” approach fails to account for the varying time demands of different consultations
- We used an initial sample set of 20 pre-agreed CCSD codes as the basis for our investigations and interviews
Testimonial
“Curzon developed the UK’s first, data-driven, value-based reimbursement fee structure. They built a transformative model that is reversing clinician attrition. Their expertise, speed, and innovative thinking have strengthened our consultant relationships“
Director of Provider Management, Leading UK Medical Insurance Provider
Curzon Approach
Benchmarking Analysis
- Comparing the client’s reimbursements on a like-for-like basis across 4 major competitors for surgeons and anaesthetists
Should-Cost Model
- Consulted surgeons and anaesthetists through interviews and survey to understand their views on fees, and used thematic analysis to map key points of consensus and divergence
- Leveraged data on the number of surgeons in different UK specialisations, NHS bands, typical procedure time,, and private practice costs to develop should cost model
CASE STUDIES
Read some of the client problems we have solved!
This Week at Curzon: Unblocking Infrastructure, Strengthening Security & Elevating Recognition
This week, we tackled the core themes of delivery resilience, cross-sector collaboration, and team celebration.
Here’s your weekly roundup:
Unblocking EV Infrastructure
Why is the UK’s EV Charger Roll‑Out Stalling?
Andrew Wilson and Edward Hunt spotlight the systemic bottlenecks behind the stalled deployment of electric vehicle charge points. Despite over 80,000 operational chargers, issues like fragmented planning, misaligned stakeholder incentives, and legacy manual processes are hampering progress.
Curzon Consulting recommends operational transformation—prioritised rollout sequencing, integrated governance, and digitised workflows—to ensure the government’s goal of 300,000 chargers by 2030 stays on track.
https://www.linkedin.com/feed/update/urn:li:activity:7341034157768093697
Cybersecurity Across Borders
Celebrating Nextcontinent’s IT Security Experts
As part of Nextcontinent “Meet the Experts” campaign, we shone a spotlight on three cybersecurity leaders within the Nextcontinent network: Jan Albert (Germany), Carlos Vidinha (Portugal), and André Rapp (Germany).
Their work is central to defending critical industries against advanced cyber threats—and reinforces our commitment to shared learning across borders.
https://www.linkedin.com/feed/update/urn:li:activity:7340678599248666624
NHS Capacity: Bricks vs Brains
Are More Hospitals Really the Answer?
Chetan Trivedi and Serban Suvagau, MBA challenge the assumption that building new hospitals is the solution to the UK NHS bed shortages. With many beds tied up in delayed discharge and new builds over budget, alternative capacity models are offering more impact:
- Day-case surgical units
- Virtual wards
- Community diagnostic hubs
- Surgical hubs
These targeted, cost-effective approaches are easing pressure without the need for major capital investment.
https://www.linkedin.com/feed/update/urn:li:activity:7340656959630512131
Celebrating Success: Healthcare Team Award
Platinum Recognition in Consultancy.uk Awards! We’re thrilled to share that our Healthcare practice has been awarded Platinum in the Consultancy.uk awards—a testament to the team’s expertise, dedication, and impact.
Huge congratulations to Chetan Trivedi, Serban Suvagau, MBA, and the entire healthcare team for earning this industry-leading accolade.
💬 Final Thought
This week’s highlights reflect our core mission: overcoming delivery challenges, empowering cross-border expertise, and championing smarter, resource-efficient solutions. From infrastructure to healthcare, Curzon Consulting stands committed to delivering systems-led change that drives real impact.
Stay connected with Curzon Consulting for more insights and updates.
📰 Subscribe for weekly insights
💼 Follow Curzon Consulting on LinkedIn
CONTACT US TO FIND OUT HOW WE CAN HELP
This Week at Curzon: Rethinking Systems for Smarter Outcomes
This week, our team explored the power of systems thinking in healthcare, defence, and finance while also celebrating connection and community through one of our prized team traditions.
Here’s your weekly roundup:
Healthcare Workforce: Beyond the GP Numbers
“We need thousands more GPs” — or do we?
Chetan Trivedi and Serban Suvagau challenge the prevailing narrative around GP shortages. While the UK government’s £29 billion NHS funding boost aims to increase the number of trained doctors, many GP graduates are struggling to find positions, even as patient demand rises.
This paradox suggests that simply increasing GP numbers may not be the optimal solution. They explore alternative models, including leveraging pharmacists, social prescribing, AI triage, and prevention-first approaches, to reshape frontline healthcare delivery.
https://www.linkedin.com/feed/update/urn:li:activity:7338895127819546624

Defence Strategy: From Vision to Execution
Reinventing the UK Defence Strategy
Bryan Clark analyses the UK’s Strategic Defence Review, highlighting significant investments: £1.5 billion for new munitions and energetics factories, procurement of up to 7,000 UK-manufactured long-range weapons, and a £5 billion investment in technological innovation, including drone and laser weapon technology. These initiatives are projected to create nearly 2,000 jobs, reinforcing the UK’s position as a ‘defence industrial powerhouse’. Bryan emphasises the need for the government to move beyond aspirational narratives and commit to specific, actionable, and quantifiable strategies to ensure effective implementation.
Check out our concise explainer (which will avoid the need to plough through the report and its references). Visit https://lnkd.in/eyapgzq2
https://www.linkedin.com/feed/update/urn:li:activity:7338506121428541440
Payments: Unpacking the Decline
“Payment Declined” — What’s Really Going On?
Sash Panda shares a personal experience of a card decline to shed light on the complexities behind payment failures. She reveals that factors beyond account balance and card status—such as the interplay between banks, networks, and merchants—can lead to false declines. With 30% of e-commerce declines being false alarms, businesses face significant revenue losses and eroded customer trust.
At Curzon Consulting, we assist financial services organisations in addressing these systemic issues to enhance customer experience and reduce unnecessary transaction failures.
https://www.linkedin.com/feed/update/urn:li:activity:7338164666629578752

Celebrating Community: Principal Dinner Highlights
An Evening of Chemistry, Conversation, and Connection, Thursday saw the latest in our Partner/Principal Dinner series, where team members Kerris Mackley, Edward Hunt, and Abhishek Roy joined Serban Suvagau for a warm and lively evening at Caravan City. The night featured thoughtful discussions about life, community, sports, and work, with a nostalgic nod to our shared chemistry roots.
A heartfelt thank you to Serban for hosting a memorable dinner, and a special shoutout to Preetesh Sood for organising the evening. It’s these moments of connection that make Curzon Consulting more than just a workplace.
💬 Final Thought
This week’s updates reflect a growing consensus: turning strategy into results demands systemic change. Whether it’s defence, procurement, or energy infrastructure, our focus remains on helping clients remove friction, unlock capability, and deliver measurable impact.
Stay connected with Curzon Consulting for more insights and updates.
📰 Subscribe for weekly insights
💼 Follow Curzon Consulting on LinkedIn
CONTACT US TO FIND OUT HOW WE CAN HELP
Excess Mortality Report
The Silent Toll: Highlighting the Surge in Non-Covid Excess Mortality Amongst the Young and Exploring Potential Causes
The Pandemic is now a memory, yet non-Covid deaths continue to rise, for reasons the UK’s top healthcare authorities are unable to explain. The UK government’s own data shows Excess Mortality spiked most significantly among young people in 2022 and 2023, and shows a substantial increase in deaths due to heart failure during the same period – in 2023 alone, 7 times more people died unexpectedly, for reasons unrelated to COVID, than died in the single worst night of the Blitz. We provide insights into the excess mortality trends, explore potential causes, and urge a proper and broader investigation of the true root causes.
Reimaging Radiology Equipment Maintenance Models - How to Enhance Cash Flow and Drive Inflation Busting Savings
With inflation at a 40-year high, how can large, multi-site operators of diagnostic equipment achieve transformative savings whilst maintaining quality?
According to Mordor Intelligence, the UK diagnostic imaging equipment market is estimated to be USD 1.1 billion in 2022 and is expected to reach USD 1.5 billion by the end of 2027.
Our research highlights, the typical profit margin on new diagnostic equipment such as a PET (Positron Emission Tomography), MRI (Magnetic Resonance Imaging), CT (Computed Tomography), Fluoroscopy, Ultrasound, X-Ray, etc... is 10-15%. However, the profit margin on maintenance contracts is > 35%.
The typical annual maintenance cost of an MRI scanner is £50,000-£70,000 and CT Scanner is £30,000-£50,000. The sum cost of all the individual maintenance contracts can mount up very quickly to several million pounds!
The actual cost of a maintenance contract can vary depending on volume discounts, hours of operation, uptime guarantees, and scope of what is included or excluded inclusions – coils, helium, etc…, along with other cost drivers.
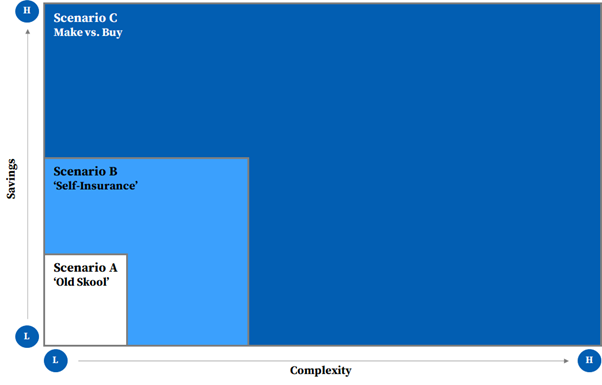
We believe there are 3 key operating models with each one driving a progressive level of savings. Scenarios B and C deliver transformative, inflation busting savings, but are the most complex to implement.
Savings vs. Complexity
Over the past few years, some organisations have turned to third-party maintenance service providers as an alternative to traditional Original Equipment Manufacturer (OEM) warranty and post-warranty support. This move has yielded substantial savings. However, that is just one solution amongst a range of others.
Scenario A – ‘Old Skool’
Under Scenario A, an organisation negotiates a full-service, gold-standard, maintenance contract with an OEM or third-party maintenance service provider.
‘Old Skool’ model can generate 10-15% savings.
Scenario A works well for a single or small hospital / diagnostic service provider business. For a large private hospital group or a diagnostic imaging service provider, this model is ‘old skool’, and worst of all, the buyer transfers significant value to the seller.
For organisations that operate a larger portfolio of diagnostic equipment, where there is a critical mass, our extensive and deep understanding of the market shows two alternative models. Both models require an open mind and can be explored together to ‘turbo-charge’ saving.
Scenario B – ‘Self-Insurance”
Under Scenario B, an organisation leverages a ‘self-insure’ model where it adoptings a risk management technique in which the company accrues a ‘pool of money’ to be used to remedy an unexpected loss from equipment breakdowns. Organisations can self-insure against equipment breakdown, and mitigate risk of large unforeseen losses by taking out implementing an excess insurance policy.
Under this scenario, an organisation buys a preventative maintenance (PM) only contract from an OEMs (Original Equipment Manufacturers) or third-party maintenance service providers, with a pre-negotiated price list for parts. The organisation pays for breakdowns as and when needed from accrued funds.
If risk is –managed appropriately, organisations can significantly enhance cash flow and savings.
‘Self-insurance’ model can generate 15-25% savings.
Scenario C – ‘Make vs. Buy’
Under Scenario C, an organisation makes a ‘make-or-buy’ decision where it chooses between setting up an in–house maintenance organisation (people, process, and systems) versus purchasing the service in part or whole from an OEM or third-party maintenance service provider.
‘Make versus buy’ model can generate 25-40% savings.
Under both Scenarios, an organisation can decide to carve-out some or all types of the diagnostic equipment for self-insurance, based on a risk assessment of service levels and uptime guarantees required per site or department.
The additional savings can be used to reinvest in new equipment, upgrades and/or drive digital transformation programmes to enhance productivity of the radiology department and improve administration, technician, clinician and patient experience.
Failure to get this right can have a material, knock-on impact on operations, patient and clinician experience, and a material loss of revenue whilst a machine is out of use.
How Can Wwe Help?
We have developed a deep understanding of the diagnostic imaging equipment market. We help clients to challenge the status quo and drive transformative benefits via the successful implementation of Scenario B and/or Scenario C.
For Scenario B – ‘Self-Insurance’, we have a methodology and proprietary analytics tools that allow us:
- accelerate the evaluation of a ‘Self-Insurance’ model
- assess financial treatment of accruals
- design options based on risk tolerance of the business
- develop a business case
- develop management information dashboard to monitor and track solution
- implement solution
For Scenario C – ‘Make vs. Buy’, we have a methodology, proprietary analytics tools and experience designing in-house operating models, that allow us:
- accelerate the evaluation of a ‘Make vs. Buy’ model
- perform maintenance demand analysis by geography
- design new Target Operation Model (TOM) options for the ‘Make’ solution
- develop a business case
- develop implementation and risk mitigation plan
- embed new TOM within an organisation
If you are interested in learning more, please contact me at chetan.trivedi@curzonconsulting.com.
CONTACT US TO FIND OUT HOW WE CAN HELP
Hip & knee implant manufacturers – The value creation opportunity
If hip and knee implant manufacturers want to stay relevant, and “move the needle” on value creation, they need to play big or go home!
An aging (ageing) population is driving absolute sales, but over the past few years, primary hip and knee procedures have become commoditised, which has resulted in margins being squeezed for both hospital providers and implant manufacturers.
Implant manufacturers have an opportunity to transform their business model, away from traditional “box shifting” product selling (driven by monthly sales targets) to a high value add, high margin managed service proposition, where multi-year partnerships are formed with hospital providers. Implant manufacturers need to provide additional services along the value chain, especially as health systems move towards value-based care models.
The Value Creation Opportunity
About the author

Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.
CONTACT US TO FIND OUT HOW WE CAN HELP
The accelerated adoption of drones in healthcare
We explore how the 2020 coronavirus crisis has accelerated the use of drones in the delivery of healthcare.
Drones in Healthcare
The commercial use of drones has steadily been gaining traction over the last decade.
The global market for medical drones was valued at USD $88.2 million in 2018. It is expected to witness 24.7% CAGR from 2019 to 2025. The UK market is anticipated to see even higher than 25% CAGR from 2019 to 2025. The global circumstances resulting from the coronavirus pandemic are likely to increase demand for unmanned aerial vehicles (UAVs) and drive the value of the drone market up even higher than forecast.
Drones have the potential to transform the delivery of healthcare. They have a large spectrum of medical uses that could be particularly valuable during this pandemic:
- Search and Rescue: searching vast areas for people in need of rescue/help in any environment
- Transport/Delivery: rapid delivery of medical supplies to rural areas between hospitals/labs or directly to the person in need
- Medical Care: remote delivery of medical advice/care

Despite wide potential applications in healthcare, the use of drones in practice has been fairly limited. Safety and security concerns have led to tight regulations on airspace. This makes it difficult to phase in drones for practical (rather than recreational) use. Drones have a bad reputation due to their potential abuse in breaching privacy, violating human rights and irresponsible use by hobbyists, particularly at airports. Consequently, only a small proportion of the potentially vast benefits offered by drones in healthcare have been realised.
COVID-19 impact on drones in healthcare
The coronavirus crisis has acted as a catalyst for the adoption and acceptance of drones in healthcare. There are two main reasons for this:
- The need to deliver medical care/supplies quickly is more urgent
- Social distancing and quarantine measures have made remotely operated systems particularly valuable
As a result of coronavirus, how has drone use changed or adoption accelerated? We’ve included some examples below.
Dutch company Avy manufactures wing drones for use in urban healthcare logistics, rural delivery of supplies, and first response emergency services. Avy responded to the pandemic by exploring the use of wing drones to transport COVID-19 samples from small municipalities to labs in larger cities. This would help contain the virus and minimise risk of the virus spreading.
We spoke to Patrique Zaman, Founder of Avy, about the healthcare challenges that Avy is trying to overcome.
This is an example of a drone company, Manna Aero, that changed their focus from food delivery to medicine delivery during the pandemic.
The Irish start-up launched their drone delivery service earlier this year, with the aim of moving road-based food delivery into the skies. Manna Aero’s trial delivery of takeaways to college students in mid-March had to be halted due to the coronavirus lockdown, but this did not deter them from switching focus to help in the crisis. The company has instead been working with the Irish Health Service Executive to deliver medicines and other essential supplies such as break and milk to vulnerable people in the rural town of Moneygall. Local GPs write prescriptions after a video consultation, which the drones deliver directly to homes. This represents a first in Ireland. Manna Aero is equipped to handle up to 100 deliveries a day, and hopes to bring trials to the UK soon.
The UK’s lockdown in 2020 triggered the government to grant permission for a UAV to deliver medical supplies across the Solent to a hospital on the Isle of Wight. This is part of a UK government project to develop a system allowing manned and unmanned aircraft to operate in the same airspace.
The UAV, developed by the University of Southampton and funded by the start-up Windracers, was given permission to fly as part of the British government’s Covid-19 response. It has a range of 1,000km and can carry up to 100kg.
Compared to the more traditional ferry, this novel approach allows faster, more frequent, and more reliable delivery of medical supplies.
The Covid-19 response has triggered a partnership between the drone delivery provider Skyports and Thales to trial the delivery of medical supplies.
The two-week pilot is backed by NHS Highland, and Argyll and Bute Council, with drones supplied by unmanned aircraft-maker Wingcopter. The delivery service will be based in Oban. It aims to ensure that isolated communities on the Isle of Mull (16km away) have access to COVID-19 tests and sufficient personal protective equipment (PPE).
This trial is a crucial milestone for unmanned aviation in the UK. It was granted as an exception to current rules by the Civil Aviation Authority.
Zipline is a US drone company that delivers supplies to rural communities in Rwanda and Ghana. In order to support the Covid-19 response in Africa, Zipline changed its focus to using drones to provide clinics with PPE and coronavirus test samples. The lightweight drones deliver to clinics up to 85km away. There are plans to use the drones to deliver supplies directly to the elderly and vulnerable who need to self-isolate.
Zipline CEO Keller Rinaudo thinks that drone deliveries could play a vital role both during the current crisis and in the coming months and years.
The Chinese government has been proactive in piloting ways to incorporate drones into their response to the coronavirus.
Drones originally designed to spray pesticides have been adapted to spray disinfecting chemicals in public spaces. Testing the use of drones to deliver of medical samples began in February, with over 20 flights per day at peak operation in Zhejiang Province. Consumer delivery of essential items has also been trialled, with e-commerce company JD developing a drone team to deliver to Anxin’s semi-isolated islands.
Future outlook
The unprecedented circumstances brought about by Covid-19 have kick-started the use of drones in new and exciting ways, but we are only scratching the surface of their full potential.
To progress, we need to learn from this pandemic and make changes that will ultimately lead to a better healthcare experience. Rather than relying on experimentation, we should pre-plan how drones can be used during disease outbreaks and make appropriate investments. Drones need to be integrated into planned health responses. In addition, coordination between the public and private sector will be crucial to overcome regulation by civil aviation authorities.
It is obvious that drones have a big role to play in the delivery of healthcare. The route to unlocking their true potential will offer exciting and rewarding opportunities in the future.
How Curzon can help
Curzon Consulting help with strategy and digital transformation. We have experience working in collaboration with companies to embed technology into their organisation. Curzon can:
- Conduct feasibility studies
- Build a business case and commercial offering
- Design the most appropriate operating model and integration plan
- Conduct a technical requirement assessment
Get in touch to find out how we can help or arrange a free virtual meeting with our Healthcare partner, Chetan Trivedi.
The authors
We can help you to improve patient outcomes with digital strategy, transformation and patient experience.
Contact us for more information or submit a request for proposal to our healthcare consulting team
Precision medicine - using data to prevent heart disease and stroke
Curzon Healthcare Lead Chetan Trivedi in conversation with Dr Rameen Shakur MD PhD (Cantab), Massachusetts Institute of Technology, Boston. We explore precision medicine, the importance of a patient centric approach to data and how medical technology is improving healthcare accessibility.
Rameen is the founder of Cambridge Heartwear and the Jansen Fellow for Cardiology and precision medicine at Massachusetts Institute of Technology (MIT). This interview was not sponsored. All views are Dr Rameen Shakur’s and not that of MIT.
Watch a highlight of our conversation below
Precision medicine and technology
Precision medicine refers to the tailoring of medical treatment to the individual characteristics of each patient.
Precision medicine does not mean the creation of drugs or medical devices that are unique to a patient, but rather the ability to sub-classify individuals into populations that differ in their susceptibility to a particular disease. And for that to occur, Rameen argues we need “not just the therapeutic arm, the diagnostic arm, but also the analytical arm to all intermingle in one.”
Rameen is the founder of Cambridge Heartwear, a medical technology and AI device manufacturer. Through novel engineering, Rameen and his colleagues at University of Cambridge fused diagnostics, and real-time delivery of data and analytics. Cambridge Heartwear aims to reduce the impact of strokes by detecting irregular heart rhythms in real-time through a pairing monitoring device and artificial intelligence algorithms. This real-time wearable ECG (electrocardiogram) device has cut the diagnosis and treatment process down from three weeks to days. Rameen explains it is also a means to measure our physiology in more granularity.
Part of Cambridge Heartwear’s goal is more integrated healthcare across primary, secondary and tertiary care. Rameen explains “once you deal with that whole process of how to manage a system to amalgamate all of those together, then you make a real inroad into what we want to call precision medicine.”
Similar to many technology companies, such as HP and Apple, Rameen built the first prototype in a shed in his back garden.
Patient centric design
What makes Cambridge Heartwear disruptive is the focus on the patient. Throughout the design process, Rameen is “very patient centric”.
This carries through to the availability and ownership of data. “It’s patient centric because if we want to get to a view of precision medicine, you have to give access to people for that data. The point is it is their data. It is their own right to actually have that data, access that data and do as they please with that data.” From the patient perspective it is a means for them to obtain specific data related to the cardiovascular system for the first time, namely the whole electricity of the heart when they’re moving around. Consequently, access to this data enables people to have an informed conversation with physicians on treatment modalities.
This focus on the patient not only applies to data but the design of the wearable itself “We wanted a wearable that would be ergonomic”. The design encompassed:
- Real-time data and analytics transmission from patient to physician across the world
- Patient experience – “we wanted a system where you can go about your daily business”
Historically many medical technology companies have adopted a male-centric approach to data and design. Rameen was mindful of gender bias in his medical technology design, stating
“the whole design was done for the anatomical differences between males and females.”
Accessibility for all is at the heart of what Rameen’s trying to achieve. He believes that coronavirus has affected healthcare by firstly highlighting the health inequalities that exist in society and secondly adopting technology to break down those barriers. “who has access has power is no longer the statement that we want to hear”. The COVID-19 pandemic has also highlighted the important role of technology to deliver information from patients’ homes to hospitals and physicians.
The future of precision medicine
We ask Dr Rameen what precision medicine could look like in the next 30 years.
“Precision medicine I hope will garner a lot of technology, innovation and discovery. In our lab, for example, we are teasing out for the first time methodologies for risk stratification for patients who may have had the genetic test.
We are getting more and more nuanced in the way we collect data. Previously, for example when we talked about disease associations, we referred to a particular subpopulation, a particular racial population… For a complete picture, one needs to know and have a whole profile of different technologies that are applicable across the board, across society. I believe what we need to do is to bring that back to society and say, let’s talk about it in the context of the population of our global population.”
I believe we will likely see more integration of digital technology with the biotech fields… I hope to see more of this sort of collaboration where novel engineering comes head to head with medical technology processes, whereby the actual information is now being stored in biological systems, having a discourse with physicians at a much more accessible point. And I think this concept which has started to happen
“It’s a very exciting time within the next five to 10 years, we’re seeing a lots of big changes”.
The concepts of portability and real time data are “something that we are very proud to work on and something that’s also of interest to us as we move to our next phase of humanity into space.” Indeed, the emergence of space travel tourism launches an opportunity to observe medical data and physiology outside of the earth’s atmosphere.
But one thing’s for certain, the aim of medical technology is not to replace humans.
“I think one of the key points about technology is we have to get away from just being a tech company. You are a human company, which is dealing with humans and for the survival of patients, we need to have all in our armoury. So I make no apology to say that we would never want to replace the physician, but rather to make that whole process a lot easier and less journey as for all involved.”
An important time for innovation in the UK
Rameen is proud of the work that UK engineers and manufacturers are doing right now. He believes that as a country
“we are very strong in artificial intelligence. We may not have previously been very vocal about that, but the proof is in the pudding. And I’m glad to say a lot of people are having the puddings!”
We can help you to improve patient outcomes with digital strategy, transformation and patient experience.
In conversation with

Dr Rameen Shakur MD PhD (Cantab), Massachusetts Institute of Technology, Founder of Cambridge Heartwear