Blockchain in healthcare: a use case
Curzon Healthcare lead Chetan Trivedi explores how Blockchain in healthcare will revolutionise the billing and payment process. This will result in the complete disintermediation of a vast administrative layer within the healthcare Provider and Payer (private insurer or public commissioner) organisation.
Consequently, Healthcare Providers and Payers will see a huge benefit through a more streamlined process of handling claims and processing payments. The process will also include various steps like checking patient insurance eligibility and coding claims.
Illustrative smart billing and payment process
The example shown below is based on an insured patient, but the process would be similar for the public sector.
1. Upfront
- Insurer and Provider enter into a Smart Contract on Ethereum blockchain
- The smart contract would be self-executing with the terms of the agreement directly written into code
- The smart contract would exist on a distributed and decentralised blockchain network
- Smart contract would permit trusted transactions and agreements to be carried out between Insurer and Provider without the need for manual intervention (Provider and Insurer), central authority, legal system, or external enforcement mechanism
- Each transaction would be completely traceable, transparent, and irreversible
- Automated invoice and subsequent payment would be triggered (i.e. self-billing) inline with pre-agreed protocols and care pathway (incorporated into the Smart Contract)
- Micropayments are triggered after each care package has been completed
- Penalties are built into the Smart Contract and are assessed automatically if Provider fails to meet quality metrics (e.g. readmission rates, infection rates, revision rates, etc.) or poor outcomes (e.g. PROM, Oxford scores)
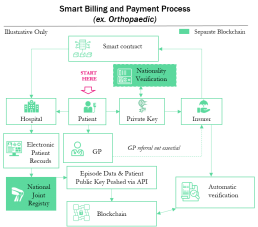

2. Ongoing
- Patient experiences symptoms (e.g. increase pain, reduce mobility etc.)
- Patient visits GP (Physician) or contacts Insurer directly (based on policy guidelines)
- Patient accesses Insurer policy automatically using Private Key
- Insurer automatically routes referral to Orthopaedic Consultant or Provider inline with policy
- Patient commences journey through care pathway (e.g. pre-op, op, post-op, discharge, follow up, etc.) and is treated by the Provider against a pre-agreed set of protocols (consultation, imaging, pathology, implant, physiotherapy, etc.) with the Insurer
- Provider feeds data into Electronic Patient Records (EPR). Standard data linked to specific non identifiable Patient Public Key and is published automatically onto the Blockchain via API
- Insurer automatically validates treatment against pre-agreed care pathway and protocols and automatically triggers payment (see Payment Triggers to left)
About the author

Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.
CONTACT US TO FIND OUT HOW WE CAN HELP
Increasing patient satisfaction through orthopaedic Enhanced Recovery Programme
The issue
- Reimbursements – Operational and commercial risk transferred from insurer to provider via fixed reimbursements
- Pain – 45%+ patients stated moderate to severe pain within 48 hours of surgery, delaying recovery
- Mobility – Physiotherapy started late usually within 24-48 hours post surgery causing delay in mobility
- Length of stay – 4-6-day length of stay resulting in marginal clinical benefit, unnecessary cost and higher infection risk
What we did
- Established one multidisciplinary team
- Developed Evidence-Based Enhanced Recovery Programme (ERP)
- Established ERP training programme
- Designed and implemented pilot ERP programme (ERP)

The results
- Reduced pain scores by 45%
- Decreased mobility times by 65%
- Shortened hospital stays by 43%
- Reduced hospital cost by 20%
- Increased patient satisfaction by 37%
An award-winning team






CONTACT US TO FIND OUT HOW WE CAN HELP
Reducing 30 day re-admissions by leveraging patient remote monitoring solution
The issue
- Colorectal surgery (related to cancer) accounted for 27% of the total case mix for a large healthcare system
- Colorectal surgery department noticed a steady increase in the number of patients returning back to the Emergency Room (ER) for non-urgent issues over a 24-month period
- 30-day readmission rates were significantly above the national average
- Based on an initial internal assessment, the hospital management and colorectal surgery department hypothesized an issue with the patient discharge process
- Established a cross-functional team to perform a root-cause analysis of the entire patient journey and flow
- Mapped the entire patient journey and flow and identified a number of improvement opportunities
What we did
- Designed a pilot study to test a new discharge process enabled by technology
- Enrolled 97 patients, focusing on younger more tech savvy profile who were open to self-managing recovery during post-operative phase
- Identified root-causes of readmissions into ER (over 78% non-emergency which could have been avoided if patients were better educated and informed during the discharge process)
- Redesigned the discharge programme with a greater focus on patient self-management enabled by smart technology
- Sent patients electronic reminders to help keep them on-track with recovery milestones
- Established post-discharge daily check-ins to track stoma output, incision photos, pain levels, bowel function, etc.
- Implemented algorithms to flag patient issues and automatically provide feedback to patients on how to self-manage or how and where to find relevant support
- Developed intelligent notifications to automatically notify clinical team members if patient at risk
- Designed and implemented a dashboard with real-time reports and analytics to help the care team understand a patient’s post-operative concerns, trajectory of recovery and ways to improve patient experience

The results
- Delivered a 72% reduction in 30-day re-admissions
- Avoided 7 ER visits which were resolved through triage via telephone consultation or outpatient clinic
- Improved patient satisfaction scores by 24% (compared to baseline pre-launch)
- Based on the success of the programme, supported client to identify other surgical programmes to roll-out similar solution
An award-winning team






CONTACT US TO FIND OUT HOW WE CAN HELP
Leveraging procurement to increase profitability of orthopaedic services
The issue
- Many suppliers (18+) resulting in reduced spend leverage
- Prosthesis selection based on supplier systems familiarity not generic technical spec
- Large cost variances for similar hip and knee systems from supplier to supplier
- Large amount of “additional” costs associated with instrumentation and loan kits
- Huge variety in ‘same’ type of hip and knee systems (7+ systems for each)
- Too many system variations (75+) resulting in staff needing to be trained on many systems/brands
- Varying published data to support clinical outcomes of implants resulting in low predictability of patent outcomes
- Huge cost-per-procedure variance impacting profitability at Orthopaedic Consultant and Hospital level
- Need to increase profitability
What we did
- Increased spend with fewer, more capable suppliers
- Established patient profiles. Use patient profiles to guide system selection
Linked into project to Care Pathways - Established minimum acceptance of prosthesis outcomes (leveraging ODEP ratings for both hips and knees)
- Established dedicated training for Orthopaedic Consultants and clinical staff
- Renegotiated with partner suppliers based on redistributed business (volumes)
- Established traffic light reporting for Ortho hip and knee (cost and compliance to agreement)
- Established a clinical advisory group to evaluate innovation and agree protocols to be followed by all Orthopaedic Consultants across the Group

The results
- Delivered 22% in annualised savings through volume leverage and brand/system standardisation
- Reduced clinical risk by only allowing 10 or 10* ODEP rated products and eliminating Orthopaedic work at low volume sites
- Increased profitability substantially which allowed the BD teams to improve NHS and PMI contract win rates
- Reduced supplier power (demonstrated appetite and willingness to shift balance of power)
- Improved patient satisfaction and outcomes by channeling more work to Orthopaedic Consultants with higher PROMs scores
- Reduced subjectivity by ensuring system selection based on patient profile
- Standardised length of stays for given procedure and patient profile
An award-winning team






CONTACT US TO FIND OUT HOW WE CAN HELP
Hospital at home: key considerations
Hospital-at-Home: an Important Component of an Integrated Care Model
New technology is arming and enabling care providers with the ability to provide seamless support to patients along the entire care continuum. Hospital-at-home care delivery models allow health systems to find the right access and intervention point for delivering targeted patient solutions
The case for change
- Unprecedented levels of total global debt to economic output (debt-to-gdp ratio) during peace time. Simply printing more money, creating more debt or throwing more money at an outdated healthcare system isn’t going to help*
- Aging population with multiple comorbidities are requiring more complex care, so patients needs to be better triaged and stratified to determine best intervention point (hospital, community, home, etc.)
- Increase in prevalence of long term chronic conditions such as hypertension, type 2 diabetes, etc. are better suited to alternative care models (e.g. community, home, etc.)
- Overcrowding of hospitals and emergency departments by patients who can been seen outside of the acute setting are causing delays for patients with higher levels of acuity to be seen earlier
- Rapid advancements in telehealth and patient remote monitoring technologies are allowing clinicians to observe and examine patients remotely, and at scale, allowing care providers to do more with less
- Consumer expectations are rapidly increasing as they demand better care experiences and improvement in quality of life
- Pressure from payers to develop high quality, less-expensive alternatives to hospital care
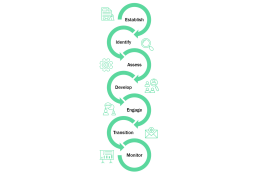
7 key considerations for a Hospital-at-Home Model
- Establish clear objectives of why your organisation is seeking to set up a hospital-at-home model. For example, is it to drive early discharge, optimise admission avoidance, diversify income stream, etc.
- Identify conditions e.g. congestive heart failure, chronic obstructive pulmonary disease, community acquired pneumonia, etc. suitable for home care delivery models based on clinical evidence. Establish patient qualification criteria for hospital-at-home programme.
- Assess patient suitability (against qualification criteria), including functional risk assessment for hospital-at-home care model. Assess patient home for safety / hazards, heating, etc.
- Develop a personalised care plan upon first care provider visit. Personalised patient care plan can be developed by a doctor, pharmacist or nurse (the latter two under the supervision of a doctor using a telehealth solution if needed).
- Engage with patients and caregivers (family members or friends). Ensure anyone supporting the patient at home is part of development of the care plan. Where appropriate, self management (with clinical support) of treatment /condition must be discussed and agreed with patient.
- Prepare patient transition from hospital-at-home programme to primary care setting. Send discharge summaries to the patient’s primary care doctor via electronic patient records system, email, etc. The transition is absolutely key and must be handled flawlessly to avoid patient “falling through cracks”.
- Monitor and provide 24/7 coverage should patient require readmission. Provide in-home diagnostic tests, medications, and equipment (if necessary). Engage with care providers in wider community as needed (e.g. palliative care services, mental health).
*Global debt has reached an all-time high of $184 trillion in nominal terms, the equivalent of 225 percent of GDP in 2017. On average, the world’s debt now exceeds $86,000 in per capita terms, which is more than 2½ times the average income per-capita. Source: International Monetary Fund (IMF), Jan ‘19
About the author

Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.